Craniocervical Junction in Craniospinal Hydrodynamics and Neurodegenerative Conditions
An essential location for preserving the cervical spine’s structural integrity is the craniocervical junction (CCJ). It is formed by the occipital region of the skull and articulates with the atlas and axis below (C1 & C2)[1].
The CCJ is easily compromised by disease and trauma, and while this compromised stability is a concern in and of itself, it can also damage neighbouring structures and result in more serious issues, especially when it comes to brain blood flow and cerebrospinal fluid (CSF) flow.
Below we describe the few major complications of a destabilized Craniocervical Junction.
More specifically, you will find information on topics:
- Internal Jugular Vein Stenosis or Compression
- Intracranial Hypertension vs. Migraines
- Long-term consequences of CSF flow inhibition
- How Common is Internal Jugular Vein Stenosis from bony processes?
- Long-term consequences of blood flow inhibition
- Myalgic Encephalomyelitis and Patients with Central Nervous Symptoms Study
1. INTERNAL JUGULAR VEIN STENOSIS or COMPRESSION
The internal jugular vein (IJV) receives venous return from the sinuses inside the cranial cavity and then drains into the subclavian vein which enters the heart.
Diseases such as idiopathic intracranial hypertension (IIH), Alzheimer’s disease (AD), Ménière disease, and multiple sclerosis are just a few of the central nervous system (CNS) disorders that have been linked to IJV stenosis [2].
A growing body of research indicates that extra-cranial venous outflow disturbances have a negative impact on the cerebral artery and venous circulation, which can lead to a variety of neurological impairments [3].
Specifically, IJV stenosis can cause decreased cerebral perfusion, altered CSF dynamics, impaired cerebral microvascular structures, and raised intracranial pressure, all leading to brain structural and functional abnormalities [4].
One study looked at internal jugular venous compression syndrome as a complication of cervical spondylosis. Out of the 92 internal jugular veins analyzed, 69 had vascular stenosis; 50.7% of these vessels were constrained by the transverse process of the atlas, and 44.9% by the transverse process of the atlas in conjunction with the styloid process (FIGURE 1). This shows that almost half of the positive cases always involve bony compression [5]. Spongylosis can mimic symptoms of amyotrophic lateral sclerosis, so knowledge of radiographic findings is necessary to differentiate the two.
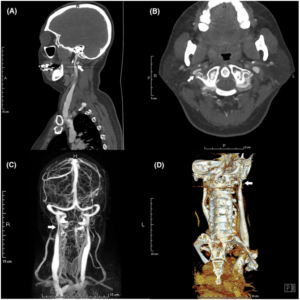
FIGURE 1: Internal Jugular Vein stenosis due to compression from transverse process of C1.
2. INTRACRANIAL HYPERTENSION vs. MIGRAINES
The internal jugular vein is not the only structure to be compressed in this manner, as it runs parallel with several other structures including nerves. The condition known as jugular outlet syndrome occurs when the neurovascular bundle exiting the jugular foramen becomes squished between the transverse process of the C1 and the styloid process of the skull as a side effect of forward subluxation of the atlanto-occipital facet joints. This frequently causes a variety of issues, including migraines, endolymphatic hydrops and intracranial hypertension.
Etiology-wise, the jugular neurovascular bundle may be compressed at the base of the skull, between the styloid process and C1, as a result of poor posture or congenitally wide C1 transverse processes or atlantooccipital misalignment [6]. Two of the aforementioned complication require focus, as one is more serious than the other. Based on their comparable symptoms, intracranial hypertension and chronic migraine might easily be misinterpreted with each other.
One can falsely rule out intracranial hypertension in the differential if all the tests and manifestations of intracranial hypertensions such as lumbar puncture opening pressure, papilledema, and sella turcica content are normal.
However, despite normal conventional imaging and lumbar puncture results, a study found several occurrences of intracranial hypertension directly due to CCJ pathology [6]. Physicians should be wary when examining a patient that has both CNS symptoms along with suspicion of CCJ disruption.
3. Long-term consequences of CSF flow inhibition
Reference [10]
| DISEASE/CONDITION | INVOLVEMENT | OUTCOMES |
| Chiari formation | Coning of brainstem | Hydrocephalus |
| Hypoplasia of the posterior fossa | Coning of brainstem | Hydrocephalus |
| Basilar invagination | Coning of brainstem | Hydrocephalus |
| Abnormal clivoaxial angle | Cervico-medullary compression | Hydrocephalus |
| Retroflexed odontoid | Cervico-medullary compression | Hydrocephalus |
| Surgical CSF shunts | Coning of brainstem | Reduced CSF flow |
4. HOW COMMON IS INTERNAL JUGULAR VEIN COMPRESSION FROM BONY PROCESSES?
Extra-cranial Internal Jugular Vein (IJV) compression is a common finding in everyday clinical practice, although it can be challenging to identify specific symptoms or syndromes. One research looked at 108 patients who underwent CT angiography, to investigate the frequency of IJV compression in the upper neck by extrinsic structures. The conclusion was that jugular vein compression was regarded as an anatomical variation and was unlikely to be pathogenic in origin.
However, styloidogenic jugular compression was deemed a newly recognized classified disease that is being recorded more frequently in recent literature. It is also known as Eagle Jugular Syndrome, styloid-induced internal jugular vein stenosis, or styloidogenic-cervical spondylotic internal jugular venous compression.
A lack of knowledge about this disease entity may result in delayed diagnosis and therapy; thus it is pertinent that more prospective research is conducted on this [7]. Similarly, another study conducted a literature review to try to find the incidence of compression by the transverse process of C1. While the clinical manifestation lacked specificity, headache, tinnitus, and sleeplessness were the most prevalent complaints.
Moreover, in 45.9% of the sample, the IJV stenosis was unilateral, and in 54.1% it was bilateral. The most often given medication for the management of these patients was an anticoagulant. Following this, 33.6% underwent endovascular therapy, and 36.9% underwent surgery. Regardless of the form of management, 72.5% had improvements in overall health while 23% of patients were reported to have complications [8].
5. Long-term Consequences of Blood Flow Inhibition
Reference [10]
** IMPORTANT NOTICE: Do not self-diagnose or jump to conclusions that you have this condition or that your vessels are compromised; And seek a Physicians diagnosis and confirmation that your vessels are involved. In fact, this statement applies to everything in this website.
| DISEASE/CONDITION | POSSIBLE VESSELS INVOLVED | OUTCOMES |
| Subclavian steal syndrome | Internal carotid – Opthalmic artery | Loss of vision Glaucoma |
| Spondylosis, stenosis, and scoliosis | Vertebral veins in epidural space | Intracranial hypertension |
| Cervical kyphosis | Internal jugular vein | Cerebral edema > Ischemia |
| Any CCJ malformation | Vertebral artery – Spinal Artery | Sensory or motor loss for nerves arising from spinal cord |
| Any CCJ malformation* | Sub-occipital cavernous sinus | Cerebral edema > Ischemia |
| Any CCJ malformation* | Vertebral venous plexus | Intracranial hypertension |
*Malformations of the CCJ include but is not limited to: atlanto-occipital assimilation, basiocciput hypoplasia, malformations of the condyle, and malformations of the dens.
6. MYALGIC ENCEPHALOMYELITIS AND PATIENTS WITH CENTRAL NERVOUS SYSTEM SYMPTOMS
The symptoms of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) include excruciating pain and unrelenting fatigue alongside neurological and immunological dysfunction. According to a research paper, patients who had Central Nervous System (CNS) symptoms typically exhibited hypermobility of the Craniocervical Junction. This was proven on magnetic resonance imaging (MRI) of the brain and the craniocervical area.
Thus, it was concluded that individuals with ME/CFS include a substantially large number of people with craniocervical obstruction and hypermobility and that many of these patients may have intracranial hypertension as well, which might account for many of the symptoms associated with ME/CFS [9]. In addition almost half these patients had cerebellar tonsil herniation on MRI (FIGURE 2).
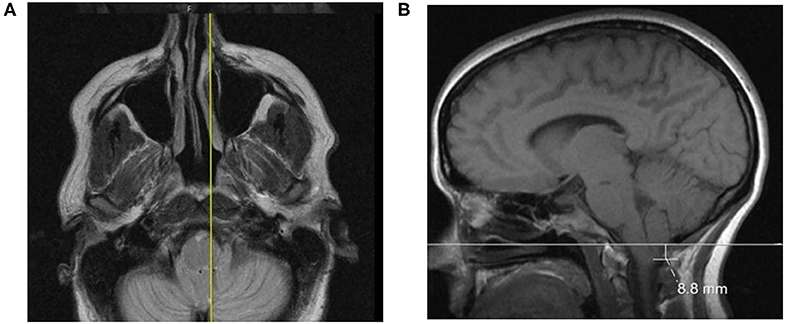
FIGURE 2. (A) A case featuring a right-sided, low-lying cerebellar tonsil; (B) The axial projection position.
REFERENCES
- Tubbs RS, Hallock JD, Radcliff V, Naftel RP, Mortazavi M, Shoja MM, Loukas M, Cohen-Gadol AA. Ligaments of the craniocervical junction: a review. Journal of Neurosurgery: Spine. 2011 Jun 1;14(6):697-709.
- Zamboni P, Galeotti R, Menegatti E, et al. Chronic cerebrospinal venous insufficiency in patients with multiple sclerosis. J Neurol Neurosurg Psychiatry. 2009;80:392‐399
- Zivadinov R, Chung CP. Potential involvement of the extracranial venous system in central nervous system disorders and aging. BMC Med. 2013;11:260
- Zhou D, Ding JY, Ya JY, et al. Understanding jugular venous outflow disturbance. CNS Neurosci Ther. 2018;24:473‐482.
- Ding JY, Zhou D, Pan LQ, Ya JY, Liu C, Yan F, Fan CQ, Ding YC, Ji XM, Meng R. Cervical spondylotic internal jugular venous compression syndrome. CNS neuroscience & therapeutics. 2020 Jan;26(1):47-54.
- Larsen K. Occult intracranial hypertension as a sequela of biomechanical internal jugular vein stenosis: A case report. Anaesthesia, Pain & Intensive Care. 2018:238-42.
- Jayaraman MV, Boxerman JL, Davis LM, Haas RA, Rogg JM. Incidence of extrinsic compression of the internal jugular vein in unselected patients undergoing CT angiography. American journal of neuroradiology. 2012 Aug 1;33(7):1247-50.
- Scerrati A, Norri N, Mongardi L, Dones F, Ricciardi L, Trevisi G, Menegatti E, Zamboni P, Cavallo MA, De Bonis P. Styloidogenic-cervical spondylotic internal jugular venous compression, a vascular disease related to several clinical neurological manifestations: diagnosis and treatment—a comprehensive literature review. Annals of Translational Medicine. 2021 Apr;9(8).
- Bragée B, Michos A, Drum B, Fahlgren M, Szulkin R, Bertilson BC. Signs of intracranial hypertension, hypermobility, and craniocervical obstructions in patients with myalgic encephalomyelitis/chronic fatigue syndrome. Frontiers in neurology. 2020:828.
- Flanagan MF. The role of the craniocervical junction in craniospinal hydrodynamics and neurodegenerative conditions. Neurology research international. 2015 Nov 30;2015.
- Rafael H. Sporadic amyotrophic lateral sclerosis. A clinical analysis. Revista del Hospital Juárez de México. 2010;77(3):224-7.
SBA Ref. Prof. AB 2023

