Craniocervical Fusion Surgery (CCF)\
Introduction to Occipital-atlantal Dissociation
Occipital-atlantal dissociation / instability / dislocation occurs due to problems at the base of the skull and the first vertebrae (atlas) (known as the occipito-atlantal joint). To prevent the neurological compromise, it’s important to fix the root cause of the problem. The management can be surgical or non-surgical.
What is Craniocervical Fusion?
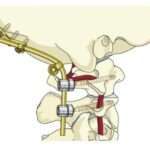
Craniocervical Fusion (CFF), also called Occipital-atlantal fusion (OAF), is used in surgical craniocervical stabilization. As the name implies, it involves fusing the base of the skull (occiput) with the atlas (C1 vertebra).
Fusion of two bones (skull to spine) is done with screws, rods, or other devices. However, in fusing the craniocervical region to restore stability in the upper cervical neck, the range of motion is affected and there is limited range of motion. As a result, it’s critical to understand when surgical intervention is necessary and when it’s not.
Indications for fusion include [1]:
1) Dislocation as a result of trauma
2) Absence of complete arch of C1
3) Congenital abnormalities of occipito-atlantal joint
4) Migration of dens in foramen magnum
5) Marked mobilization at C1 or C2 which is not reducible. This might injure the cord and cause neurological deficits.
Again, it’s important to note that the craniocervical fusion (CFF) can reduce the mobility at the joint and that there’s always a risk of non-union.
Pre-Operative Craniocervical Fusion Investigations
In cases of hereditary or congenital connective tissue disorders, either isolated or part of a syndrome, genetic testing might be recommended. But the most common cause of instability is trauma.
In all cases, irrespective of the cause, before going for surgery, it is essential to obtain thin slice CT Scans. The scan should encompass the occipital bone from above the external occipital protuberance to at least the C-4 cervical spine level. Coronal and sagittal reconstructions as well as axial images are required. Some centers also recommend a 3D CT-Scan.
Upright MRI is recommended in the flexed and extended position to it remove any suspicion of any neural compromise. The MRI tells the extent of instability, and is also really helpful in cases of any previous posterior fossa surgeries [2].
Baseline lab work-up, as required in any other surgery, including full blood count, basic metabolic profile, and basic coagulation work-up is needed.
Craniocervical Fusion Surgical Options
The choice of fusion depends on many factors including individual characteristics, subjacent connective tissue disease, bony density, involvement of posterior cervical elements, surgeon expertise and technology availability. Therefore, the caregivers must discuss these factors with the operating surgeon beforehand, understand all the options, and then decide the most suitable one [3].
The options for occipito-cervical fusion include [1]:
- Keel plate occipital cervical fusion
- Occipital condyle-C1 polyaxial screws
- Occipital-C1 trans-articular screws
The significant details of these options are discussed below:
1. Keel Plate Occipital Cervical Fusion
The thickness of occipital bone is measured beforehand using CT scan to determine screw-length for occipital screws. The patient is usually positioned prone [1,4,5]. Technique [4]:
Step 1: A plate is placed over the occiput below the external occipital protuberance. For this, the occiput bone is dissected up to the external EOP and laterally as far as needed to accommodate the plate. The plate is placed in the midline of the occiput.
Step 2: Once the plate is in position, the location of the central screw entry point is marked.
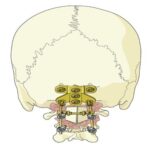
Step 3: The area of central cranial screw is then drilled.

Step 4: A screw of appropriate length is then passed through the pre-drilled hole.

Step 5: After placement of the first screw, remaining screws are placed through the same technique. Care is taken while placing lateral screws as occiput bone is thinner laterally.
Step 6: Cervical screws are then placed. C1 lateral mass screws, C2 pedicle/ pars/ laminar screws or C3 laminar screws can be inserted, depending on the level of fixation that is required.
Step 7: After correct alignment, rods are placed between the occipital and cervical screws to fuse occiput and cervical bones. Wires are used when plates and rods are not available.
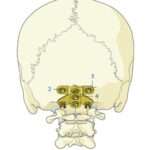
2. Occipital Condylar Polyaxial Screws
The technique only differs from the above technique in the way that polyaxial screws are placed in the occipital condyles rather than a plate which are then connected to screws at lower levels via rods. This technique provides a greater surface area for fusion, can be used in patients who have undergone posterior fossa craniectomy, and prevents risk of intracranial damage. However, it is not applicable in all patients due to condylar variability [1].
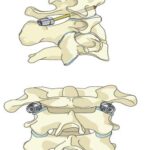
3. Occipital-C1 transarticular screws
The technique only differs from the above technique in the way that 28–32 mm cannulated lag screws are used. They are entered from C1 lateral mass to exit at occipital condyle [1].
Post-Operative Craniocervical Fusion Care
Patients are allowed to sit the same evening after the operation, and are allowed to mobilize depending on the degree of neurological deficit. A halo vest is used in patients with severe C1 fractures or impaired bone healing for 8-12 weeks. Otherwise, a Miami-J collar can be used for immobilization. Patients are then followed with periodical X-Rays in clinics usually at 6 weeks, 3 months, 6 months, and 1 year, but can be followed earlier as well.
For SOME STUDIES ON post-fusion outcomes, keep scrolling down.
REFERENCES
- Greenberg MS. Handbook of Neurolsurgery. 9th edition. New York: Thieme; 2020.
- Menezes AH. Craniocervical fusions in children: a review. Journal of Neurosurgery: Pediatrics. 2012 Jun 1;9(6):573-85.
- Pingarilho AR, de Melo PM, Elbabaa SK. Postoperative Immobilization following Occipitocervical Fusion in the Pediatric Population: Outcome Evaluation and Review of Literature. Pediatric Neurosurgery. 2018;53(2):81-8.
- Lehman R, Riew D, Schnake K. Occipitocervical fusion (screw fixation). surgeryreference.aofoundation.org. Accessed January 8, 2022. https://surgeryreference.aofoundation.org/spine/trauma/occipitocervical/c0-fractures/occipitocervical-fusion-screw-fixation
- Ashafai NS, Visocchi M, Wąsik N. Occipitocervical fusion: an updated review. New Trends in Craniovertebral Junction Surgery. 2019:247-52.
SBA Reference: Neurosurgeon F.S. Jan. 2023.
Congress of Neurological Surgeons’ Cost Analysis of Spine Surgery
“The objective of the study was to demonstrate the variability in outcomes and cost at population level and individual patient level for patients undergoing spine surgery for degenerative diseases. A total of 1454 patients were analyzed. There was significant improvement in patient-reported outcomes at postoperative 1 year (P < .0001). For patients demonstrating health benefit at population level, 12.5% of patients experienced no gain from
surgery and 38% failed to achieve minimal clinically important difference.
The study’s conclusion is that spine treatments that on average are cost-effective may have wide variability in value at the individual patient level. The variability demonstrated here represents an opportunity, through registries, to identify specific care that may be less effective, and refine patient-specific care delivery and indications to drive overall group-level treatment value.
Understanding value of spine care at an individualized as well as population level will allow clinicians, and eventually payers, to better target resources for improving care for non-responders, ultimately driving up the average health for the whole population.” Reference
USA Neurosurgeon Dr. Fraser Henderson’s Long-Term Study
“Dr. Fraser Henderson describes the results of his ongoing, long-term study following patients who received craniocervical fusions to correct instability as a treatment method for “cervical medullary syndrome”, which includes syndromes such as Chiari, dysautonomia and more. These results are reported five-years out of initial fusion surgery and prove very promising as a means of treatment in patients whose symptoms stem specifically from cranial instability.” Reference Video. Reference Article

