MAIN STABILIZERS OF THE CRANIOCERVICAL JUNCTION
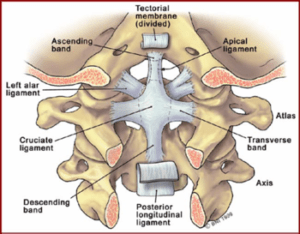
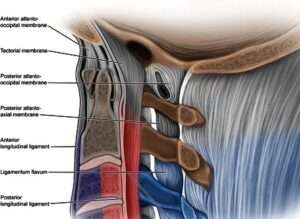
Tectorial membrane
The tectorial membrane, a superior extension of the posterior longitudinal ligament, extends to the anterior margin of the foramen magnum and covers the caudal portion of the clivus. It is a strong, wide band of fibrous tissue that runs from the occipital bone of the skull down to the axis (C2). The tectorial membrane is the major craniocervical stabilizer. It helps to stabilize the craniocervical junction by limiting excessive flexion and extension of the head and neck.
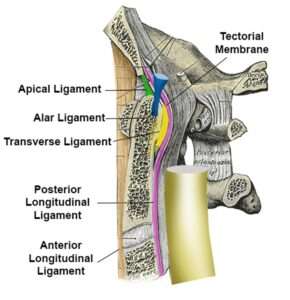
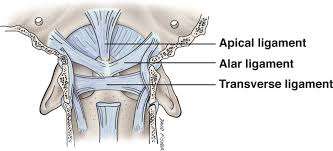
Alar ligaments
The pair of alar ligaments that attach the axis (C2) to the base of the skull. Their work is to hold your head onto your neck. Alar ligaments are short, thick bands of tissue that run from the side of the dens to the occipital bone. They are important in limiting rotation of the head and neck. Together with the transverse ligament, these ligaments are primary stabilizers of the craniocervical junction.
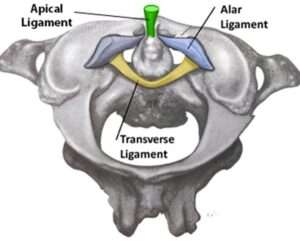
Transverse ligament of the atlas
This transverse ligament of the atlas is arguably the most important ligament in your body. It is the thickest and the strongest of the craniocervical junction ligaments. It is a primary stabilizer and one of the most important stabilizers of the craniocervical junction. It limits anterior subluxation / dislocation of the atlas and provides stability to the craniocervical junction. It holds the odontoid process (the bony projection of the axis that sits in the right of the atlas) in place and prevents it from compressing the spinal cord.
Cruciate / Cruciform Ligament This ligament consists of two bands: the transverse ligament of the atlas and the longitudinal band that form the shape of a cross. It is an important ligament that holds the posterior dens of C2 in articulation at the atlanto-axial joint. It provides additional support to the odontoid process and helps prevent excessive motion of the craniocervical junction. Ultimately, the cruciate ligament of the atlas prevents abnormal movements of the atlanto-axial joint. The longitudinal bands prevent hyperflexion and hyperextension of the occipital bone, and hold the transverse ligament of the atlas in a normal position.
LIGAMENTS THAT PLAY A ROLE IN LIMITING FLEXION OR EXTENSION
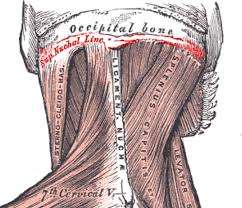
Nuchal ligament (ligamentum nuchae)
This is an upward continuation of the supraspinous ligament and extends from the bony projection off every vertebra called the spinous process (of the C7 vertebra) attaching to the back of the occipital bone. It limits too much bending of the neck.
Anterior atlanto-occipital membrane (AAOM)
The anterior atlanto-occipital membrane is a slim structure attaches the front side of the atlas bone (C1) to the foramen magnum (the big hole in the base of your skull). It serves to provide stability to the craniocervical junction in a number of ways including: restricts excessive forward movement (anterior translation), limits atlanto-occipital extension, it provides support to the atlanto-occipital joint, it assists in load-sharing between the anterior column of the spine and it protects vital structures that lie posterior to the atlas (C1) including the spinal cord and brain stem.
VERY LITTLE INVOLVEMENT, IF ANY PART, IN CRANIOCERVICAL INSTABILITY:
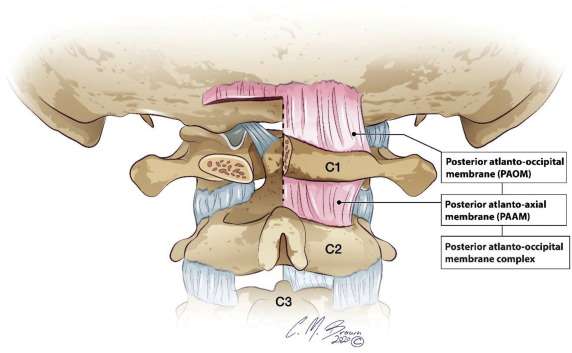
Posterior atlanto-occipital membrane (PAOM)
It is believed that this membrane plays very little part in the stability of the atlanto-occipital joint. The main function is to separate the suboccipital muscles from the cervical spinal cord and the contents of the posterior cranial fossa, allowing for the movement of the head and neck.
Apical ligament of the Dens
This ligament extends from the tip of the odontoid process to the basion. It probably offers little significant contribution to craniocervical junction stability.
Important Note:
With the exception of the alar ligaments and transverse ligament of the atlas, there is quite a bit of contradicting medical studies on the biomechanics and ligament’s roles in stability; and so take this information with a grain of salt!
To help diagnose some conditions of the craniocervical junction, there are a number of measurements that are used by doctors, specifically radiologists, on images of different modalities to help to decide whether you have craniocervical instability or not.
MEASUREMENTS USED TO HELP DIAGNOSE CRANIOCERVICAL INSTABILITY
1. Atlantodental interval (ADI)
The lateral atlantodental interval is the horizontal distance between the lateral cortex of the dens and the medial cortex of the lateral masses of the atlas. (See figure 2). The normal value is 3.4 mm in either the right or left atlantodental interval. (note: other sources state 3mm). Read more.
2. Basion dens interval (BDI)
BDI is the distance from the lower part of the basion and the tip of the dens. Doctors use this measurement to check for injuries in the neck area. The basion is a point at the base of your skull, and the dens is a projection of a bone in your neck. Normal values for adults are less than 12 mm on an XRay and less than 8.5 mm on CT . In children, greater than 10 mm may suggest atlanto-occipital injury. Reference. Note: *Some Neurosurgeons consider ≥ 10 mm in adults as pathological. Read more.
3. Basion-axial interval (BAI)
BAI is the horizontal distance between the basion and the backside of the axis in the midline side view (figure 5). It normally measures <12 mm. A measurement of >12 mm represents CCI. Read more.
4. Power’s Ratio
Power’s Ratio is the distance measured from the tip of the basion to the posterior arch of C1 divided by the distance from the opisthion to the anterior arch of C1 (figure 6). A ratio <1 is considered normal. If this ratio is >1, then the anterior atlanto-occipital dissociation should be suspected. Read more.
5. Clivo Axial Angle (CXA)
CXA is the angle between the Clivus and the backside of the Dens is approximately 155o (figure 7) ranging between (135–179°). CXA of <135° is considered abnormal. Note: Many medical articles indicate CXA normal range in neutral is 145 – 160 degrees. Read more.
6. Grabb Oakes Line (GOL)
Grabb Oakes is the distance from the dura perpendicular (upright) to the line drawn from basion to the back of the lower part of C2 vertebra (Figure 8). The Dura is a protective layer that covers the Spinal Cord and the Brain. A GOL measurement of ≥9 mm suggested a high risk of ventral brainstem compression. Read more.
7. Chamberlain’s line
Chamberlain’s line is a line drawn from the backside surface of the hard palate to the tip of the opisthion (backside of the foramen magnum). It is used to measure the distance of how much the odontoid tip extends above this line. If the tip of the dens extends > 3 mm above this line it means there is basilar invagination. Note: Some medical articles indicate that > 5mm is abnormal.
The table below shows CCJ measurements, an indication of type of craniocervical instability, and the suggested biomechanical issues associated with craniocervical junction abnormalities:
Note: New studies are now being published regarding normal CCJ in dynamic imaging (i.e. flexion and extension). This is relevant as there are patients that have normal CCJ measurements in neutral, but abnormal measurements in flexion and extension, causing spinal cord and/or brainstem compression in flexion and/or extension.
| Measurement | Aids in Diagnosis of | Indicative of horizontal, vertical, or rotational instability | Normal | Borderline | Pathological | Suggests the biomechanical failure of what ligaments and/or other parts of anatomy |
| ADI | Atlanto-axial Instability. Abnormal ADI is also indicative of Atlanto-occipital instability | Horizontal Instability (C1-C2 moves in horizontal plane). | ≤ 3mm | NA | > 3mm | ADI of 7 mm suggests rupture or incompetence of the transverse ligament of the cruciate ligament, and an ADI of 10 mm suggests loss or incompetence of the alar ligaments as well. However, if the transverse ligament is intact, the ADI is normal despite the presence of alar ligament incompetence. |
| BDI | Atlanto-occipital dissociation | Horizontal instability (C2 odontiod process and body moves anterior to basion in horizontal plane) | <12mm in adult<10mm in children | NA | >12mm in adult>10mm in children | BDI of greater than 12mm suggests there is anterior displacement of the posterior margin of the odontoid peg and body of the axis relative to the basion. And this result from complete or partial disruption of the tectorial membrane and bilateral alar ligaments. |
| BAI | Atlanto-occipital dissociation | Horizontal Instability | <12mm (on radiographs)8.5mm to 26mm (on CT images) | NA | >12mm (on radiographs)>26mm (on CT images) | Basion-axial interval or BAI is considered abnormal when there is anterior displacement of 12 mm or more or posterior displacement of 4 mm or more between the basion and posterior C2 line. This can be caused by partial or complete disruption of the tectorial membrane and bilateral alar ligaments. |
| Chamberlain line | Basilar invagination | Vertical instability -the skull and C1 moves down as one unit with respect to the spine (cranial settling) resulting in upward translocation of the odontoid process | <3mm | NA | >3mm | The tip of the dens should be below this line, if it is above this line by more than 3mm, this is suggestive of basilar invagination. Which could be due to developmental softening of the bones of the skull base (in congenital conditions) or due to incompetent transverse ligament (in acquired conditions). Note: Some articles reference 5mm, not 3mm. |
| CXA | Ventral (anterior) brain stem compression. | Horizontal Instability/ (Horizontal translation of the cranium and horizontal tilting of the odontoid) | >135° | NA | <135° | CXA angle of less than 135 (more acute CXA) creates a fulcrum by which the odontoid deforms the brainstem (causing medullary kinking). This usually results from thickening of the posterior ligament due to inflammation of joint lining (pannus). |
| Grabb Oakes Line | Ventral brainstem compression | Horizontal InstabilityThe dens of C2 moves backward in horizontal plane | <9mm | NA | ≥9mm | GOL of 9mm or more suggests that the dens of C2 bone is malpositioned or unstable (encroaching into the upper spinal canal), or there is thickening of the capsule on the Dens (pannus) |
| Power’s Ratio | Anterior atlanto-occipital dissociation | Horizontal instability | <1 | NA | >1 | Powers ratio of more than 1 suggest that there is weakening or rupture of transverse ligament. Or there is congenital cervical vertebral fusion syndromes that may predispose to AOD by creating a fulcrum-like effect. |
| Translational BDI | Craniocervical instability | Horizontal Instability | 7.1 mm in flexion and 8.4 mm in extension | NA | >7.1mm in flexion and >8.4mm in extension. | Translational BDI of >7.1mm in flexion and >8.4mm in extension may suggests complete or partial disruption of tectorial membrane and bilateral alar ligaments. |
| Translational BAI | Craniocervical instability | Horizontal Instability (there is a dynamic translation between the basion and the odintoid). | 1 mm | NA | 2mm or more | A dynamic translation between the basion and the odontoid of >1 mm may be suggestive of CCI. And could be caused by partial or complete disruption of tectorial membrane and bilateral alar ligaments. |
| Rule of Spence | Injury to the transverse atlantal ligament (TAL) | Horizontal Instability | <6.9 mm | 6.9 mm | >6.9 mm. (>8.1 mm is considered more accurate according to recent studies) | If the combined projection of the lateral masses of the atlas is more than 6.9 mm beyond the lateral masses of the axis, an injury to the transverse ligament is likely. |
| Degree of rotation in rotational AAI | Torticollis (atlantoaxial rotatory subluxation) | Horizontal Instability | 40° | 45° | > 45° | If the transverse ligament is unusually lax or weak, facet interlock may occur even with rotation of <45°. And this suggest that alar ligament disruption is the mechanism by which rotatory subluxation occurs. |
DISCUSSION
The craniocervical region is a complex area that relies on bony and ligamentous integrity to maintain its stability. Any abnormality that involves these components (especially the ligaments) results in craniocervical instability. This condition is investigated through a neurosurgeon or orthopaedic physician and one of the steps in examination is by applying different measurements that were shown above on various radiologic imaging.
Below we provide evidence-based answers to some questions by patients of CCI, their families, or other stakeholders in this regard.
1. What muscles can the patient strengthen to support their head and neck if they have abnormal ADI measurement?
Abnormal ADI indicates there is craniocervical instability (Atlanto-occipital dissociation or Atlantoaxial Instability), and part of it conservative treatment is physiotherapy which involves training of deep and superficial cervical flexors (muscles).
Deep cervical (neck) flexor muscles are Rectus Capitus Anterior, Rectus Capitus Lateralsi, Longus Capitis, Longus Coli, and Longus Cervicis. Superficial neck flexors include Sternocleidomastoid and Scalene anterior.
A physiotherapy source that many EDS patients reference is Living Life to the Fullest with Ehlers-Danlos Syndrome by Kevin Muldowny
A small subset of CCI patients have found help with Orthobiological Injections although much more research in regarding cervical spine injections needs to be conducted.
If conservative treatments fail or if CCI is diagnosed as severe and causes neurological compromise, Craniocervical Fusion (CCF) surgery may be the management option for some patients.
See other Treatment / Management Options
2. Does the apical ligament have any mechanical significance? Does a partially torn apical ligament cause basilar invagination?
The apical ligament is a small and weak ligament that extends from the tip of odontoid process of C2 and attaches to the basion. It does not contribute significantly to the stability of craniocervical junction. And it is absent in 20% of people. Therefore, complete or partially torn apical ligament does not cause basilar invagination.
3. Is there any truth to some physicians’ claims that the majority of craniocervical instability, regardless of (Oc-C1 or AAI) is due to injury/laxity primarily in the transverse and alar ligaments?
This statement is true to some extent because the majority of CCI is due to ligamentous injury that involves the transverse and alar ligaments which are the most important ligaments for stability of the atlanto-occipital articulation in addition to the tectorial membrane. CCI can also occur when there are abnormalities with the bones of the craniocervical junction like in occipital condyle fracture.
4. If we classify measurements of CCI into “vertical” instability and “horizontal” instability, would there essentially be different “biomechanical failures” for vertical and horizontal craniocervical instability?
No, because some biomechanical failures (for example incompetent transverse ligament) can result in both horizontal and vertical instability.
REFERENCES
- Nicholson, L.L., Rao, P.J., Lee, M. et al. Reference values of four measures of craniocervical stability using upright dynamic magnetic resonance imaging. Radiol med 128, 330–339 (2023). https://doi.org/10.1007/s11547-023-01588-8
- Henderson F Sr, Rosenbaum R, Narayanan M, Mackall J, Koby M. Optimizing Alignment Parameters During Craniocervical Stabilization and Fusion: A Technical Note. Cureus. 2020 Mar 2;12(3):e7160. doi: 10.7759/cureus.7160. PMID: 32257703; PMCID: PMC7112711.
- Offiah, C.E., Day, E. The craniocervical junction: embryology, anatomy, biomechanics and imaging in blunt trauma. Insights Imaging 8, 29–47 (2017). https://doi.org/10.1007/s13244-016-0530-5
- Kasliwal MK, Fontes RB, Traynelis VC. Occipitocervical dissociation-incidence, evaluation, and treatment. Curr Rev Musculoskelet Med. 2016 Sep;9(3):247-54. doi: 10.1007/s12178-016-9347-6. PMID: 27255101; PMCID: PMC4958379.
- Lacy J, Bajaj J, Gillis CC. Atlantoaxial Instability. [Updated 2023 Feb 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519563/
- Crook TB, Eynon CA. Traumatic atlantoaxial rotatory subluxation. Emergency Medicine Journal 2005;22:671-672.
- Meza Escobar LE, Osterhoff G, Ossendorf C, Wanner GA, Simmen HP, Werner CM. Traumatic atlantoaxial rotatory subluxation in an adolescent: a case report. J Med Case Rep. 2012 Jan 23;6:27. doi: 10.1186/1752-1947-6-27. PMID: 22269577; PMCID: PMC3275470.
- Park MS, Moon SH, Kim TH, Oh JK, Nam JH, Jung JK, Riew KD. New Radiographic Index for Occipito-Cervical Instability. Asian Spine J. 2016 Feb;10(1):123-8. doi: 10.4184/asj.2016.10.1.123. Epub 2016 Feb 16. PMID: 26949467; PMCID: PMC4764523.
- Tectorial Membrane Injury.
SBA would like to thank to Dr. E. Deng as the main contributor for this article.

