Blood Flow and Craniocervical Instability (CCI)
Below is a brief summary of the relationship between the craniocervical junction and blood flow. It includes:
- The Craniocervical Junction
- Key Arteries & Veins of the Head and Neck
- Internal Jugular Vein Stenosis / Compression
- Vertebrobasilar Insufficiency and Craniocervical Instability
- Long-term consequences of blood flow inhibition
- Conservative Management Suggestions*
1. The Craniocervical Junction
An essential location for preserving the cervical spine’s structural integrity is the craniocervical junction (CCJ). It is formed by the occipital region of the skull and forms a joint with the atlas and axis below (C1 & C2) Reference.
The CCJ is easily vulnerable to disease and trauma, and while craniocervical stability is a concern in and of itself, it can also damage neighbouring structures and result in more serious issues, especially when it comes to cerebral blood flow and cerebrospinal fluid (CSF) flow. Below we describe the few major complications of a de-stabilized craniocervical junction.
2. Key Arteries & Veins of the Head and Neck
The brain and brainstem require a constant delivery of nutrients and oxygen from the blood vessels that travel through the neck. The main two blood vessels that send blood to the brain are the vertebral artery and the carotid artery. The vertebral artery travels up through the outer portion of the bones in the neck and through the atlas bone (the top bone of the spine). The carotid artery travels deep in the neck and passes directly in front of the atlas bone.
Blood that travels to the brain also has to leave the brain effectively. The largest blood vessel that drains the brain is the internal jugular vein (IJV). The internal jugular vein also passes directly in front of the atlas bone (C1) on its way down the neck.
3. Internal Jugular Vein Stenosis / Compression and Craniocervical Abnormalities
The internal jugular vein (IJV) receives venous return from the sinuses inside the cranial cavity and then drains into the subclavian vein which enters the heart.
Diseases such as idiopathic intracranial hypertension (IIH), Alzheimer’s disease (AD), Ménière disease, and multiple sclerosis are just a few of the central nervous system (CNS) disorders that have been linked to IJV stenosis. Reference
A growing body of research indicates that extra-cranial venous outflow disturbances have a negative impact on the cerebral artery and venous circulation, which can lead to a variety of neurological impairments. Reference Specifically, IJV stenosis can cause decreased cerebral perfusion, altered CSF dynamics, impaired cerebral microvascular structures, and raised intracranial pressure, all leading to brain structural and functional abnormalities. Reference
One study looked at internal jugular venous compression syndrome as a complication of cervical spondylosis. Out of the 92 internal jugular veins analyzed, 69 had vascular stenosis; 50.7% of these vessels were constrained by the transverse process of the atlas, and 44.9% by the transverse process of the atlas in conjunction with the styloid process (FIGURE 1).
This shows that almost half of the positive cases always involve bony compression. Reference Spondylosis can mimic symptoms of amyotrophic lateral sclerosis, so knowledge of radiographic findings is necessary to differentiate the two.
Blood flow traveling out of the brain through the jugular vein may cause issues. When the brain cannot correctly drain, pressure can build in the brain cavity. This can lead to migraines, idiopathic intracranial pressure and hydrocephalus. If left long enough, there is some evidence showing that this can lead to long term neurodegeneration.
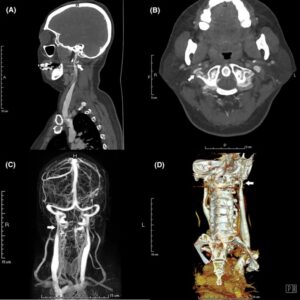
Figure 1. Neuroimaging features of right IJVS induced by the C1 transverse mass.
4. Vertebrobasilar Insufficiency and Craniocervical Instability
Craniocervical Instability or a misalignment of the craniocervical junction (the joints between the skull and the top of the spine) may cause pressure and tension on these blood vessels, reducing their blood flow.
When blood travelling to the brain is diminished reduced, it can cause problems in the brain. Vertebrobasilar insufficiency is when the vertebral arteries do not deliver enough blood to the brainstem and the back of the brain.
Vertebrobasilar insufficiency can lead to vision problems, dizziness, loss of balance or coordination and numbness in the hands and feet.
Reduced blood flow to the brain can also diminish brain activity over time. Without proper blood flow, brain function and concentration are impaired. The longer that blood flow carrying oxygen and nutrients to the brain is reduced, the more difficult it becomes to think clearly and have the brain work at its best.
5. Long-term consequences of blood flow inhibition [10]
** IMPORTANT NOTICE: Do not self-diagnose or jump to conclusions that you have this condition or that your vessels are compromised; And seek a Physicians diagnosis and confirmation that your vessels are involved. In fact, this statement applies to everything in this website.
|
DISEASE/CONDITION |
VESSELS INVOLVED |
OUTCOMES |
|
Subclavian steal syndrome |
Internal carotid – Opthalmic artery |
Loss of vision |
|
Spondylosis, stenosis, and scoliosis |
Vertebral veins in epidural space |
Intracranial hypertension |
|
Cervical kyphosis |
Internal jugular vein |
Cerebral edema > Ischemia |
|
Any CCJ malformation |
Vertebral artery – Spinal Artery |
Sensory or motor loss for nerves arising from spinal cord |
|
Any CCJ malformation* |
Sub-occipital cavernous sinus |
Cerebral edema > Ischemia |
|
Any CCJ malformation* |
Vertebral venous plexus |
Intracranial hypertension |
*Malformations of the CCJ include but is not limited to: atlantooccipital assimilation, basiocciput hypoplasia, malformations of the condyle, and malformations of the dens.
6. Conservative Management Suggestions*
*Note: discuss options with your treating physician(s) before trying the following suggestions
- Exercise at least 30 minutes a day, such as walking, aqua-fitness or walking in water (the pressure of the water pushes more blood up and into the brain and the water is gentle on the body/joints). If you are bedbound and able, try doing 5 minutes of gentle movements every few hours, even if moving your fingers and toes to a favorite song. If you cannot do #1, we completely understand!
- Drink enough water daily (i.e. 11 cups daily for women and 15 cups for men)
- Daily gentle neck stretches in the morning and nighttime as recommended by a PT or Upper Cervical Chiropractor
- Proper Body Postures as recommended by an Occupational Therapist
- Visit Upper Cervical Chiropractic NUCCA, Atlas-Orthogonal or Blair.
- Visit an Osteopath.
- Visit a Registered Massage Therapist who specializes in Lymphatic massage.
- Visit a Physiotherapist (PT) – preferably one that specializes in head and neck trauma, or Ehlers Danlos Syndrome.
- Diet – Eat foods that improve blood circulation like 1 oz (30 g) dark chocolate, beet juice, spinach, 1 cup berries and limit salt intake.
- Talk to your physician about appropriate medication options.
SBA Note: The Role of the Craniocervical Junction in Craniospinal Hydrodynamics and Neurodegenerative Conditions, summary by Prof. AB 2023

