Basion-dens interval (BDI)
A key radiology measurement to check stability between the skull and the upper neck, specifically to evaluate how well the skull is aligned with the upper cervical spine, particularly the C2 vertebrae. It helps detect conditions where the skull may be settling downward or separating from the spine, which could place pressure on the brainstem or spinal cord.
BDI is due mainly to atlanto-occipital dissociation (AOD), which can include dislocation and subluxation, multiple research papers have been conducted on the subject. It is a key radiological measurement for craniocervical instability, often used together with BAI Basion-Axial Interval.
Is BDI a widely utilized radiology measurement?
Yes, basion-dens interval (BDI) is a widely utilized measurement by neurosurgeons around the world.
What part of my body involves the basion-dens interval (BDI)?
The basion-dens interval (BDI) is the distance between two points in your neck: the basion and the tip of the dens. Doctors use this measurement to check for injuries in the neck area. The basion is a point at the base of your skull, and the dens is a projection of the C2 vertebra.
What can disturb the regular basion-dens interval (BDI)?
Any condition causing atlanto-occipital dissociation can also affect the BDI. The atlanto-occipital joint is the link between the first vertebrae (atlas) and the base of the skull (occiput).
Common causes include:
High-energy trauma: This type of injury is most commonly caused by high-energy trauma with hyperextension of the skull, such as car accidents.
Age: Children and young adults are more frequently affected due to specific anatomical predispositions. An atlanto-occipital dislocation occurs five times more commonly in children than adults.
What are the typical symptoms associated with abnormal BDI?
Patients with an abnormality of the BDI could experience the following symptoms:
-
-
-
- Motor or sensory neurological deficiencies: This can include weakness or loss of sensation in the arms or legs.
- Cranial nerve deficiencies: This can affect vision, hearing, and facial movements.
- Cervical-medullary syndrome: This can cause various symptoms, such as difficulty swallowing, hoarseness, and weakness in the arms or legs
-
-
Diagnostic Imaging to examine BDI

CT Scan or upright Cone Beam CT Scan (CBCT) is ideal to measure BDI, as it is more accurate than other imaging modalities.
BDI measurement can be obtained on MRI, however the measurement is not accurate as MRIs are best for visualizing soft tissues, not bony structures; none-the-less, MRIs can provide a “thumb guide” to roughly assess BDI.
Lateral XRay imaging can also be used for measuring BDI, however, like MRI, the quality of the image is low and the measurement should be used as a preliminary exam to determine if further investigation using CBCT/CT is advised.
Last but not least, supine or imaging in neutral position can be helpful in assessing or ruling out atlanto-occipital dissociation (AOD), however, upright dynamic flexion-extension imaging can be most helpful.
What does the radiology measurement Basion-dens Interval (BDI) aim to help rule out?
Atlanto-occipital dissociation (AOD) (i.e. base of skull to first vertebrae) injuries include both atlanto-occipital dislocations and atlanto-occipital subluxations (i.e. instability).
Although dislocations are usually fatal, subluxations are rarely fatal but occur with less frequency than dislocations.
How do Radiologists measure BDI?
The basion-dens interval (BDI) is the distance between the basion and the tip of the dens, used in the diagnosis of atlanto-occipital dissociation injuries.
Normal values for adults are less than 12 mm on an XRay (a less precise imaging modality) and less than 8.5 mm on CT . In children, greater than 10 mm may suggest atlanto-occipital injury.
Some Neurosurgeons consider ≥ 10 mm in adults as pathological/abnormal.
What treatment options are available for abnormal BDI?
This depends upon the severity and cause of the abnormality. The treatment options include:
-
- Quick diagnosis: It is essential for your physician to quickly diagnose the injury to minimize the risk of further harm to you.
- Immobilization: Your physician may use a particular device, such as a neck brace, to keep the head and neck still to prevent further injury.
- Surgery: In some cases, surgery may be needed to fuse the bones in the neck and head together to provide stability.
- Breathing support: In severe cases, patients may need help breathing, so they are admitted into an ICU where their doctor may use a tube to help them breathe.
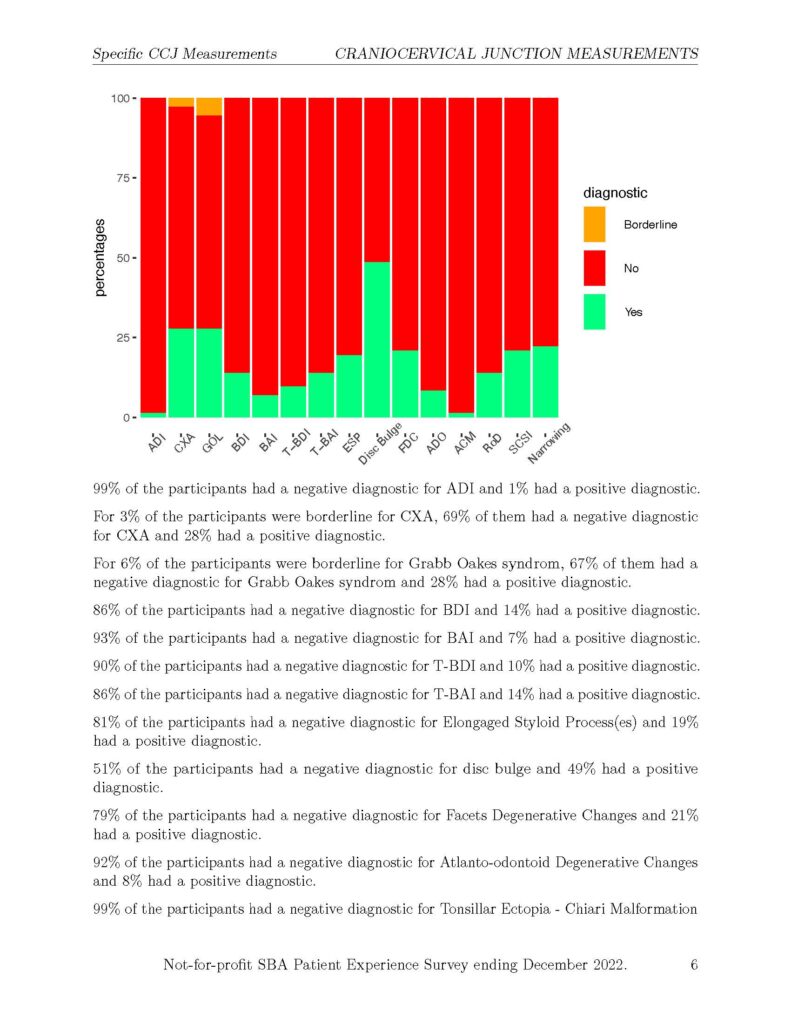
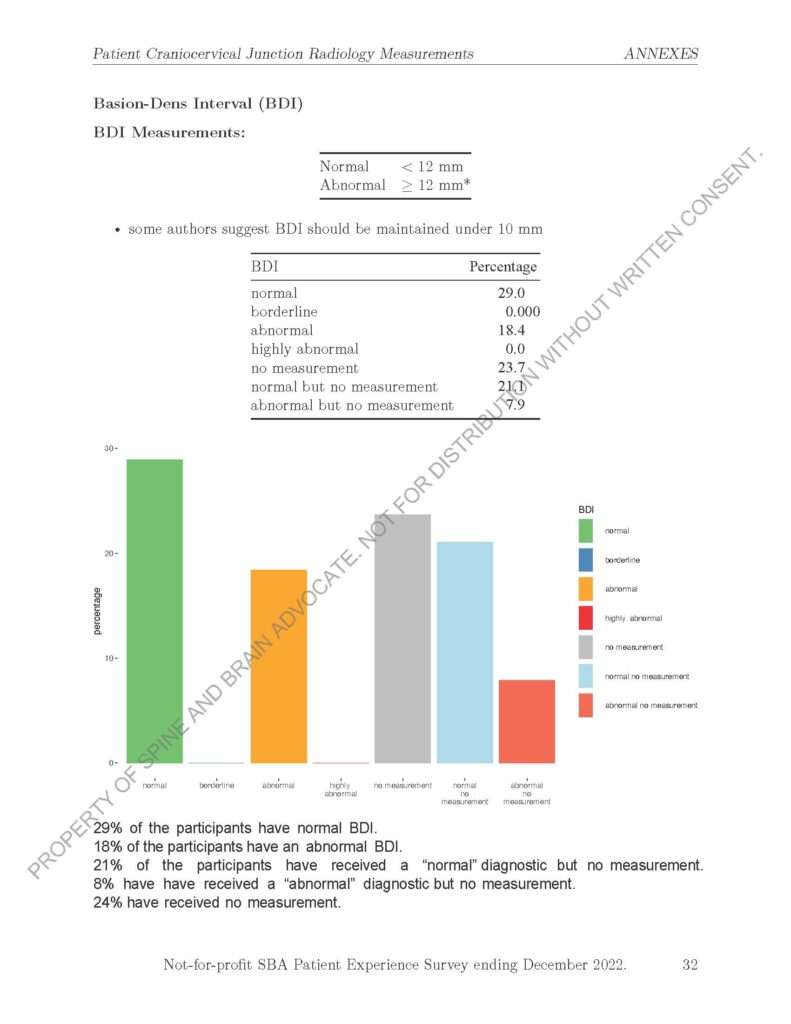
The following chart is from SBA’s 2nd Radiology Report Summary of Outcomes ending December 2022. 14% of the participants had an abnormal BDI measurement and 10% had an abnormal t-BDI measurement.
In the CCJ Patient Experience Summary Report ending December 2022 reported, 18% reported they had an abnormal BDI measurement and 8% reported they were told they had an abnormal BDI measurement but did not receive the measurement.
BDI REFERENCES
- Hacking C. Basion-dens interval | Radiology Reference Article | Radiopaedia.org [Internet]. Radiopaedia. [cited 2023 Apr 30]. Available from: https://radiopaedia.org/articles/basion-dens-interval
- Hacking C. Basion-axial interval | Radiology Reference Article | Radiopaedia.org [Internet]. Radiopaedia. [cited 2023 Apr 30]. Available from: https://radiopaedia.org/articles/basion-axial-interval-1
- Hosalkar HS, Cain EL, Horn D, Chin KR, Dormans JP, Drummond DS. Traumatic atlanto-occipital dislocation in children. J Bone Joint Surg Am. 2005 Nov;87(11):2480–8.
- Vachata P, Bolcha M, Lodin J, Sameš M. Atlanto-occipital dissociation. Rozhl V Chir Mesicnik Ceskoslovenske Chir Spolecnosti. 2020;99(1):22–8.
- Atlanto-axial instability (AAI): What you need to know [Internet]. Massachusetts General Hospital. [cited 2023 Apr 30]. Available from: https://www.massgeneral.org/children/down-syndrome/atlantoaxial-instability-aai
- Holy M, Szigethy L, Joelson A, Olerud C. A Novel Treatment of Pediatric Atlanto-Occipital Dislocation with Nonfusion Using Muscle-Preserving Temporary Internal Fixation of C0-C2: Case Series and Technical Note. Journal of Neurological Surgery Reports. 2023 Jan;84(01):e11-6.
- Lepard JR, Reed LA, Theiss SM, Rajaram SR. Unilateral atlantooccipital injury: A case series and detailed radiographic description. Journal of Craniovertebral Junction and Spine. 2022 Jul 1;13(3):344.
- Wathen C, Ghenbot Y, Chauhan D, Schuster J, Petrov D. Management of Traumatic Atlantooccipital Dissociation at a Level 1 Trauma Center: A Retrospective Case Series. World Neurosurgery. 2023 Feb 1;170:e264-70.
- García-Pérez D, Panero I, Lagares A, Gómez PA, Alén JF, Paredes I. atlanto-occipital dislocation with concomitant severe traumatic brain injury: A retrospective study at a level 1 trauma centre. Neurocirugía (English Edition). 2023 Jan 1;34(1):12-21.
Important Note: Having access to medical information is a powerful thing and an important part of advocating for your healthcare. However, this website should never replace advice from your physician who understands your specific medical history and is trained to care for patients.
If you have any suggestions or see any errors on this page, please contact us.
SBA Thanks Professor of Medical Education, Dr. A. Bohari for contributing to this page.